Key Takeaways
- Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure primarily used to treat individuals with major depressive disorder (MDD) who have not responded to traditional therapies.
- TMS is also recognized for its expanding applications in treating conditions such as OCD and migraines, and is being researched for several other disorders.
- The therapy offers minimal side effects compared to traditional medications, and insurance coverage for TMS is becoming more widespread.
- While TMS has many advantages, it’s not suitable for everyone, including those with certain implants or a history of seizures.
Table of Contents
- Understanding TMS Therapy
- Primary Beneficiaries: Individuals with Treatment-Resistant Depression
- Expanding Applications: Beyond Depression
- Advantages Over Traditional Treatments
- Considerations and Limitations
- Insurance Coverage and Accessibility
- Conclusion
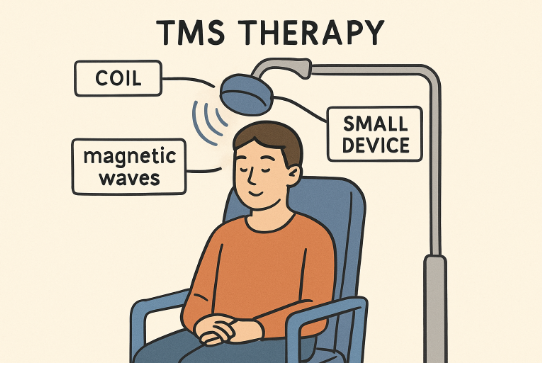
Understanding TMS Therapy
Transcranial Magnetic Stimulation (TMS) is a breakthrough, non-invasive treatment that uses focused magnetic fields to stimulate nerve cells in targeted areas of the brain. It’s most often used for individuals struggling with major depressive disorder (MDD), especially those who have not found adequate relief with medications or psychotherapy. The procedure involves positioning an electromagnetic coil on the scalp, which sends painless magnetic pulses to regulate brain activity responsible for mood.
For individuals seeking clinically proven healing alternatives, TMS therapy in St. George offers both hope and effective results. This innovative therapy is transforming the landscape for individuals who have exhausted traditional options and are seeking new possibilities for wellness. The virtually pain-free, outpatient nature of TMS also makes it an attractive treatment for people with busy lifestyles or those who want to avoid the side effects of medication.
Primary Beneficiaries: Individuals with Treatment-Resistant Depression
The group that has seen the most significant benefit from this technology comprises patients with treatment-resistant depression. These are individuals who have not responded to multiple trials of antidepressant medications or conventional talk therapy. According to Harvard Health, roughly 50% to 60% of patients with this kind of depression experience a reduction in symptoms with TMS therapy, and about one-third go on to achieve complete remission. As the therapy is non-systemic—meaning it does not circulate through the bloodstream—it also avoids many of the side effects commonly associated with medications used to treat depression.
Expanding Applications: Beyond Depression
While major depressive disorder remains the leading indication for TMS, its uses are growing. The FDA has approved TMS for conditions like obsessive-compulsive disorder (OCD), migrainous headaches, and to aid in smoking cessation. Furthermore, ongoing research suggests TMS could also benefit people with generalized anxiety disorder (GAD), post-traumatic stress disorder (PTSD), and even chronic pain syndromes. As evidence mounts, more individuals from diverse backgrounds are finding the therapy helpful, broadening its impact far beyond its original purpose.
Advantages Over Traditional Treatments
For those battling the distress of persistent mental health symptoms, one of the most significant advantages of TMS is its minimal side effect profile. Traditional antidepressant medications can cause an array of systemic side effects, including weight gain, drowsiness, sexual dysfunction, and gastrointestinal issues. TMS, by contrast, is typically limited to mild scalp discomfort or a low-grade headache during or after treatments—side effects that are generally well-tolerated and quickly subside.
Another benefit is that TMS does not require anesthesia, so patients can return to normal activities, such as driving or working, immediately after a session. The lack of cognitive impairment also makes TMS preferable for those concerned about memory or attention issues related to some other mental health treatments.
Considerations and Limitations
Despite its promise, TMS isn’t universally suitable. Individuals with metallic implants in the head or neck, such as cochlear implants, deep brain stimulators, or certain aneurysm clips and stents, may face contraindications because magnetic fields can interfere with the operation of these devices. Additionally, those with a personal or family history of seizures should discuss the risks with their healthcare provider, as TMS does carry a slight risk of seizure.
It’s also essential for patients to undergo a thorough evaluation to determine if TMS is appropriate for their specific symptoms, medical history, and treatment goals. Open communication with a mental health care provider ensures the most effective, safe, and personalized use of TMS.
Insurance Coverage and Accessibility
As the clinical evidence and demand for TMS have increased, so has insurance coverage across the United States. Most major insurance providers now include TMS as a covered benefit for individuals with treatment-resistant depression, provided they meet specific criteria, such as proof of unsuccessful attempts with other therapies. Access and approval do still vary, so patients should verify benefits and discuss potential costs and authorizations with their insurance company upfront.
The increasing accessibility of TMS means that more individuals in need can receive innovative treatment without facing significant financial barriers. This expansion is crucial for communities aiming to improve mental health outcomes.
Conclusion
Transcranial Magnetic Stimulation delivers meaningful benefits for people who have not achieved relief from traditional depression treatments and offers valuable advantages in terms of safety and convenience. As the applications of TMS continue to grow, more individuals facing different mental health challenges stand to gain from this cutting-edge therapy. With minimal side effects, broadening accessibility, and promising research avenues, TMS is shaping the future of comprehensive, non-invasive mental health care.